You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
My MRI Images, Brain and Internal Auditory Canal (IAC)
- Thread starter Eric N
- Start date
More options
Who Replied?haha yah it is pretty cool it also feels kinda weird to be looking at your own brain.Cool stuff! I wish I knew more about what I am seeing though.
Anyways all I can do is try to compare them with the acoustic neuroma mri images found on google.
Are we watching wisdom in action? Joke aside, I hope everything went okay? Did you do this scan only to rule out any acoustic neuroma or did the test give other answers as well? Was it done on your initiative or did a physician motivate you to do it?
Joke aside, I hope everything went okay? Did you do this scan only to rule out any acoustic neuroma or did the test give other answers as well? Was it done on your initiative or did a physician motivate you to do it?
 Joke aside, I hope everything went okay? Did you do this scan only to rule out any acoustic neuroma or did the test give other answers as well? Was it done on your initiative or did a physician motivate you to do it?
Joke aside, I hope everything went okay? Did you do this scan only to rule out any acoustic neuroma or did the test give other answers as well? Was it done on your initiative or did a physician motivate you to do it?Are we watching wisdom in action?Joke aside, I hope everything went okay? Did you do this scan only to rule out any acoustic neuroma or did the test give other answers as well? Was it done on your initiative or did a physician motivate you to do it?
Well to rule an acoustic neuroma and maybe signs of a stroke and no I had to motivate physician to write me a referral
 they said it was not necessary but it might make me less worried and help with habituation.
they said it was not necessary but it might make me less worried and help with habituation. For the time being everything seems normal, I just hope any small tumors weren't missed because they did not use contrast.
How do they inject contrast when it comes to the head? Did you go inside a classic tubular MRI machine or was it customized for your type of scan? I've done some MRI-orthography scans in my life and each time the injection has been placed by what seemed like a qualified specialist. I was surprised to see that the procedure was kinda circumstantial. I had one done in my shoulder earlier this year, prior to my last surgery in November.
The Red Viper
Member
- May 11, 2016
- 384
- Tinnitus Since
- March 15, 2016
- Cause of Tinnitus
- Current Theory: Neck injury (Tendonitis @ trap/SCM junction)
Poyraz
Member
- Mar 23, 2016
- 234
- Tinnitus Since
- February 2016
- Cause of Tinnitus
- Benzos, Stress, Anxiety, Loud Music, Jaw Problems. Who knows
The problem with MRIs (and even CAT scans) is that they cannot see inside the inner ear. They can only show the structure of the semicircular canals and auditory channel (outer ear). To really understand T, there needs to be a better imaging process that can look "inside" the cochlea.
The problem with MRIs (and even CAT scans) is that they cannot see inside the inner ear. They can only show the structure of the semicircular canals and auditory channel (outer ear). To really understand T, there needs to be a better imaging process that can look "inside" the cochlea.
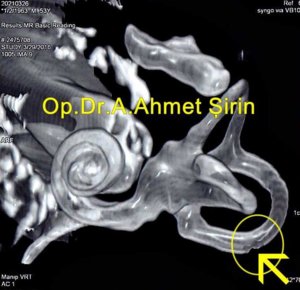
I think they already found it. I found this one from a Turkish ENT's Facebook rTMS fan page.
Attachments
The Red Viper
Member
- May 11, 2016
- 384
- Tinnitus Since
- March 15, 2016
- Cause of Tinnitus
- Current Theory: Neck injury (Tendonitis @ trap/SCM junction)
I think they already found it. I found this one from a Turkish ENT's Facebook rTMS fan page.
Nice... that's some fine detail. I wonder if they can see hairs, etc.
I think they already found it. I found this one from a Turkish ENT's Facebook rTMS fan page.
This is really a good find. Apparantly Washington and Duke have been working on a technique called 3D Magnetic Resonance Microscopy. The results of the scan can be used to create a 3D image of the cochlea. More on it here; http://oto2.wustl.edu/cochlea/mrmeth.htm
It seems that it is possible to image the cochlea, just not worth it...
@Cityjohn just wanted you to see this post. Not sure if it helps with getting more information on the inner ear. See the few posts above
Thanks this is a really good post.
The Red Viper
Member
- May 11, 2016
- 384
- Tinnitus Since
- March 15, 2016
- Cause of Tinnitus
- Current Theory: Neck injury (Tendonitis @ trap/SCM junction)
This is really a good find. Apparantly Washington and Duke have been working on a technique called 3D Magnetic Resonance Microscopy. The results of the scan can be used to create a 3D image of the cochlea. More on it here; http://oto2.wustl.edu/cochlea/mrmeth.htm
It seems that it is possible to image the cochlea, just not worth it...
Thanks this is a really good post.
Just curious, why do you think it's not worth it? I liken it to the increase in power of a particle accelerator. The more energy in the collision, the more particles that can be discovered.
Just curious, why do you think it's not worth it? I liken it to the increase in power of a particle accelerator. The more energy in the collision, the more particles that can be discovered.
What I meant was it appears that the technique has already been developed in 1994 but apparently there hasn't been a sufficient reason for doctors to implement it. This may be because it is expensive, requires specialist expertise, and as we all know for some reason tinnitus isn't considered a life threatening condition...
I've posted this a couple of other places, but there seems to be on-going interest.
There is work on imaging techniques to view the inner ear at the cellular level in order to understand what is damaged. See, for example,
http://biomedicaloptics.spiedigitallibrary.org/article.aspx?articleid=1392727
http://proceedings.spiedigitallibrary.org/proceeding.aspx?articleid=1691511
Additionally, at least one attempt is underway to design an endoscope for inner ear imaging
http://www.researchposters.com/Posters/COSM/COSM2015/F010.pdf
If they can get this worked out, it will be a big step forward to be able to correlate hearing tests and patient reports with imaging of the inner ear and to attempt to develop hearing tests that can distinguish inner ear damage.
Much of this work seems to be done by a relatively large group at Mass Eye and Ear and Harvard. It's not as sexy as stem cells or gene therapy but this - along with drug delivery methods - seems necessary to better target therapies.
There is work on imaging techniques to view the inner ear at the cellular level in order to understand what is damaged. See, for example,
http://biomedicaloptics.spiedigitallibrary.org/article.aspx?articleid=1392727
http://proceedings.spiedigitallibrary.org/proceeding.aspx?articleid=1691511
Additionally, at least one attempt is underway to design an endoscope for inner ear imaging
http://www.researchposters.com/Posters/COSM/COSM2015/F010.pdf
If they can get this worked out, it will be a big step forward to be able to correlate hearing tests and patient reports with imaging of the inner ear and to attempt to develop hearing tests that can distinguish inner ear damage.
Much of this work seems to be done by a relatively large group at Mass Eye and Ear and Harvard. It's not as sexy as stem cells or gene therapy but this - along with drug delivery methods - seems necessary to better target therapies.
What I meant was it appears that the technique has already been developed in 1994 but apparently there hasn't been a sufficient reason for doctors to implement it. This may be because it is expensive, requires specialist expertise, and as we all know for some reason tinnitus isn't considered a life threatening condition...
This should definitely be developed! Something to advocate for along with Join the Dots. A push for improved testing and ways to better delineate specific pathology in specific types of tinnitus.
@Steve , just calling your attention to the imaging test for the cochlea (see above).
- Aug 21, 2014
- 5,052
- Tinnitus Since
- 1999
- Cause of Tinnitus
- karma
The Red Viper
Member
- May 11, 2016
- 384
- Tinnitus Since
- March 15, 2016
- Cause of Tinnitus
- Current Theory: Neck injury (Tendonitis @ trap/SCM junction)
I've posted this a couple of other places, but there seems to be on-going interest.
There is work on imaging techniques to view the inner ear at the cellular level in order to understand what is damaged. See, for example,
http://biomedicaloptics.spiedigitallibrary.org/article.aspx?articleid=1392727
http://proceedings.spiedigitallibrary.org/proceeding.aspx?articleid=1691511
Additionally, at least one attempt is underway to design an endoscope for inner ear imaging
http://www.researchposters.com/Posters/COSM/COSM2015/F010.pdf
If they can get this worked out, it will be a big step forward to be able to correlate hearing tests and patient reports with imaging of the inner ear and to attempt to develop hearing tests that can distinguish inner ear damage.
Much of this work seems to be done by a relatively large group at Mass Eye and Ear and Harvard. It's not as sexy as stem cells or gene therapy but this - along with drug delivery methods - seems necessary to better target therapies.
It seems in the first link that they "sacrificed" the mice
 . However, the two-photon technique could be used in conjunction with the Harvard endoscope to image the cochlea of a living human being. From my cursory reading, what they did was cut a skin flap around the tympanic membrane, following by insertion using a small wire into the round window area. As the two-photon technique link also describes a contrast agent, a clear image of damaged cochlear cells (of whatever kind) could be more pronounced. *This is assuming that the contrast agent reacts differently to "normal" cells than it does to damaged ones.
. However, the two-photon technique could be used in conjunction with the Harvard endoscope to image the cochlea of a living human being. From my cursory reading, what they did was cut a skin flap around the tympanic membrane, following by insertion using a small wire into the round window area. As the two-photon technique link also describes a contrast agent, a clear image of damaged cochlear cells (of whatever kind) could be more pronounced. *This is assuming that the contrast agent reacts differently to "normal" cells than it does to damaged ones.In addition to the imaging, I also see the endoscope as a way to better target drug delivery as well as stem cells.
The Red Viper
Member
- May 11, 2016
- 384
- Tinnitus Since
- March 15, 2016
- Cause of Tinnitus
- Current Theory: Neck injury (Tendonitis @ trap/SCM junction)
I agree. I found an article on middle ear endoscopy from 2014 that suggests some of the difficulties encountered with the ET:Let me just add that I don't like the approach where a slit is made to fold the ear drum flap down. I would much prefer an approach where the endoscope is slid up the Eustachian tube (assuming it could be done without breaking it).
from: http://emedicine.medscape.com/article/860570-overviewIn 1989, Kimura introduced the concept of endoscopy of the middle ear through the eustachian tube orifice.[3] This technique has not met with the same clinical success as transtympanic endoscopy because of the small image size provided by the scope, difficult orientation, and poor illumination. In a recent study, 25% of endoscopy attempts through the eustachian tube orifice were aborted because of local irritation, bleeding, thick mucus, and/or blocked view by bony spicules.
Presumably the inner ear would be more difficult. However, one would think that the ability to do such imaging would get better as technology improves.

 Member
Member