https://www.healtheuropa.eu/treatment-for-deafness/88286/
Could hair cell regeneration be a treatment for deafness?
28th September 2018
A treatment for deafness could be on the horizon, as a European study investigates the possibility of inducing regeneration of the inner ear cells.
Researchers have proposed to use embryonic
stem cells as a platform for in vitro inner ear studies to potentially be a treatment for deafness. Deafness due to disease, ageing, or birth defects is caused by the loss of hair cells in the inner ear, which is the structure responsible for the detection of equilibrium and sound. Currently, deafness is a progressive and irreversible condition in humans, with the typical treatment to be the use of hearing aids.
Utilising hair cells from stem cells.
Dr Andrew Jarman, project coordinator, explains: "our approach relies on a different methodology that allows for the first time, the production of large numbers of hair cells. ″
The scientists of the EU funded
GRNHairCell project proposed to use embryonic stem cells (ESCs) as a platform for in vitro inner ear studies. ESCs establish an alternative and powerful approach to, generate unlimited numbers of hair cells in a simple culture dish without the use of animals.
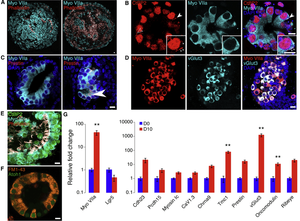
Dr Aida Costa, who performed the work, used the three proteins which control the hair cell development in the embryo – Atoh1, Pou4f3 and Gfi1.
Through genetic manipulation of ESCs to activate expression of these transcriptional regulators, a direct and robust conversion of stem cells into a hair cell phenotype was successfully achieved. "A simple in vitro culture system gave us the opportunity to investigate how these proteins work together in a network to induce the formation of hair cells." Said Costa.
Using the in vitro culture system, researchers were able to provide vital insight into the dynamics of hair cell regeneration. Atoh1 had been the main protein undergoing intense research, as it is a key player in identifying the regeneration of lost hair cells in patients with deafness. However, Atoh1 demonstrated limited regenerative capacity, indicating that other factors are implicated in the process. During the GRNHairCell study, Dr Costa identified Gfi1 as a switch to hair cell commitment and a contributor to Atoh1 transcriptional activity. Moreover, analysis of gene expression and protein-DNA binding activity unveiled important information on the function of these regulatory factors.
What is the clinical significance?
The molecular structure in which Gfi1 is able to change Atoh1 and Pou4f3 transcriptional activity is most definitely of great scientific importance. Costa highlights the fact that from a clinical perspective "it is also important to test this particular combination of transcription factors in animals with damaged inner ears to see if we can reverse the damage. ″
Jarman concludes: "although there may be no immediate clinical application of the GRNHairCell study results, the gained knowledge brings us a step closer to comprehending the process of inner ear development and exploiting it in the therapy of deafness.
Identifying the key aspects in hair cell regeneration could potentially lead scientists to establish therapeutic approaches and even find a treatment for deafness.

 Member
Member